Royal Family Birth Weight Challenge
You can use this link to make a donation to March of Dimes.
You can use this link to read all the March of Dimes post that will be added to the Blind Canine Sports site between November 5 and December 24. In 2005, Eric was born on November 5 and release from the NICU to come home on December 24.
Thank you for visiting the Royal Family Birth Weight Challenge fund raising page to help us celebrate our son’s 18th birthday. Eric has agreed to the sharing of his story to support March of Dimes and to provide hope for others who might be experiencing a similar situation.
To provide some background, the following is an excerpt from a book Mike has started and probably will never finish. Note: Mike often collectively refers to his wife, Wendy, daughter, Taylor, and son, Eric, as The Royal Family Boat crew.
Filling The Boat
Now is a good time to step back and review the events that took place to fill the boat and complete The Royal Family Boat Crew.
Big Sister Taylor’s Birth

On November 30, 2002, Taylor’s labor and delivery was typical, resulting in a healthy baby girl. She did arrive three weeks early, which caught Wendy and I a bit off guard. We missed our last Antenatal class, also called birth and parenting class, we were attending to help us to get ready for labor, birth, breastfeeding and caring for a newborn baby. The idea was going to class would help Wendy and I be more confident as the birth approached. Taylor must have been getting bored with the class, because regardless if Wendy and I were ready or not, we were busy in the labor and delivery room on the night we were to attend our last class.
While I referred to Taylor’s birth as typical, it did not go without causing some commotion. My guide dog, Cody, and I were both in the labor and delivery room with Wendy during the 14 hours of labor and the birth. Once the word spread around the hospital that Cody was in the delivery room, a parade of doctors, nurses, volunteers, the nurse teaching the Antenatal class and even some fellow students attending the birth and parenting class would stick their heads in to try and catch a glimpse of the black Labrador Retriever that was peacefully laying in the corner. Cody was waiting to learn if a boy, girl or hopefully a puppy, would soon be added to the family.
Ready Or Not Here Comes Eric
Three years in the future, on Nov. 5, 2005, Eric was born. Anything but typical could be used to describe Eric’s birth.
It was late in the day on November 4 when Wendy and I returned home after my physical therapy session following my second knee surgery. Wendy mentioned that she had been feeling a bit funny all day. A few hours later, when the pain had not stopped, I insisted she call David and Karen, our friends who lived nearby, to take her to the hospital or I was going to call an ambulance. A couple of hours later, after some scrambling by David and Karen, David was at our house with sleeping Taylor, Karen was back home with their daughter, and I was sitting in the corner of the labor and delivery room with Wendy. I had no guide dog with me this time, just a pair of crutches.
Wendy had a reaction and her heart rate spiked when some medicine was injected in an attempt to slow down the labor. The last thing the nurses said before wheeling Wendy’s entire bed out of the room to take her to surgery for an emergency cesarean delivery was “just leave him” in reference to me sitting in the corner.
Welcome To The NICU
The next conversation I had with a nurse was letting me know my son was born and he was in the Neonatal Intensive Care Unit (NICU), and that Wendy was recovering well and would be returning to the room shortly. We soon learned that newborn babies who need intensive medical care are often put in a special area of the hospital called the NICU. The NICU has advanced technology and trained healthcare professionals to give special care for the tiniest patients. Most babies admitted to the NICU are preterm (born before 37 weeks of pregnancy), have low birth weight (less than 5.5 pounds), or have a health condition that needs special care. Eric was born at 29 weeks of pregnancy and weighed three pounds and four ounces.
While still waiting for Wendy to be returned to the room, the nurse also informed me that Eric had been placed in an incubator and put on oxygen as he was experiencing brief stops in breathing (apnea). She encouraged me not to worry as only a minimal amount of oxygen was being used. The nurse probably thought my greatest concern would be Retinopathy of Prematurity (ROP). The use of too much oxygen in treating premature babies can cause vessels to grow abnormally and cause blindness. In fact, blindness was the one condition that Wendy and I knew something about already.
As promised, Wendy shortly arrived back to the room. Then, we took more than the normal nursing staff to be transferred to the NICU to go see our son as Wendy was being rolled in her bed and I was being pushed in a wheelchair. I now joke, upon seeing Wendy and my arrival into the NICU, Eric decided he better stay in the NICU for seven weeks to allow us time to recover before returning home with us.
Thank You Grandma
For the first few weeks that Eric was in the NICU we were blessed to have my mom come stay with us. This allowed Wendy to recover from the cesarean delivery and Taylor had Grandma readily available for multiple daily trips to the park. Wendy did not have to go to the store, while I could enjoy Mom’s home cooking between spending several hours a day using the CPM machine. CPM, also called continuous passive motion, is a device that is used to gently flex and extend the knee joint. The CPM machine was being used after the surgery to manipulate my leg to break up scar tissue. Because I had next to no range of motion, it was necessary to use the machine to cause the knee joint to slowly bend to improve range of motion and decrease pain. Wendy also was more than willing to allow Mom to assist me in conquering the learning curve associated with the use of the toilet riser I received upon being released from surgery. Lucky for me, the pain medicine took some edge off and reduced any embarrassment of needing such assistance. Plus, my mom had already seen my cute caboose before when changing my diapers some 37 years earlier.
As Eric got stronger and Wendy, Taylor and I got more self-sufficient, My stepdad, Bill, came to spend Thanksgiving with us and. after our feast. it was time for Mom and Bill to return to Colorado. The Royal Family Boat Crew needed to start preparing for Eric to come home.
Preparing For Eric’s Homecoming
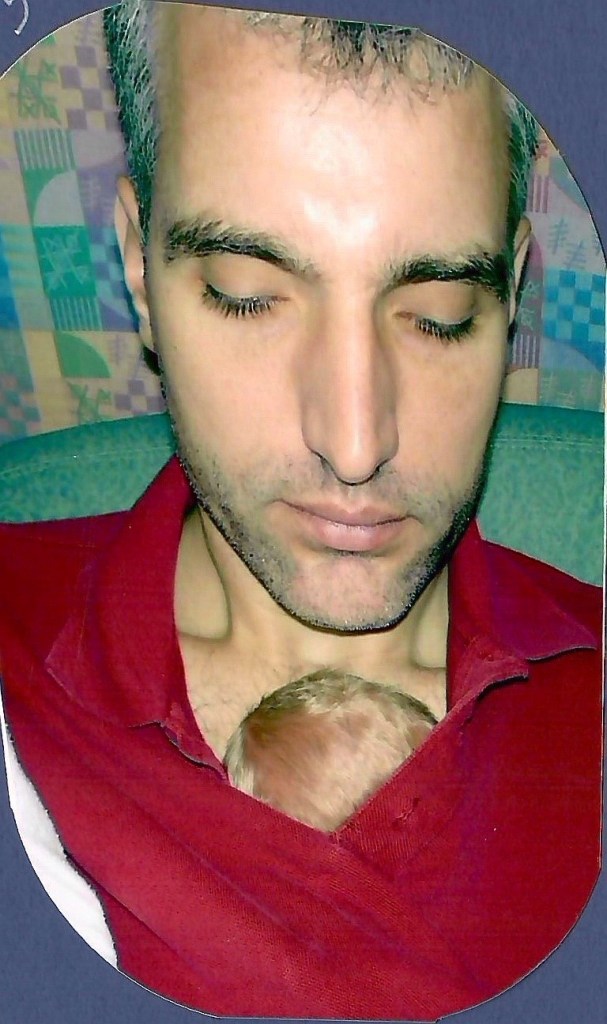
In 2005, a typical December weekday would start with Wendy dropping me off at work and Taylor attending daycare and Wendy going to the NICU. At lunch, someone from my office would give me a ride to the hospital and verbally guide me to the NICU, while my second guide dog, Syrus, was learning to heal next to my left crutch. Some of the skills learned during a winter of Alpine ski racing came in handy as the person guiding would walk in front of me and have me follow their voice then tell me to turn left or turn right as I recall these were all easy and slow turns. Once in the NICU, I would spend some skin-to-skin time with Eric by laying his small body on my chest under my shirt. The NICU nurses encouraged this skin-to-skin, or ’kangaroo’ care, which involves holding your baby against your bare chest to provide extra warmth and promote bonding. Wendy would return Syrus and me to work after our lunchtime visit, and she would head back to the NICU to stay with Eric. At the end of the workday, someone from work would drop me off at The Woodlands Sports Medicine Centre for physical therapy. Wendy would get Taylor from daycare and then would pick me up after physical therapy for another Eric visit. Lastly, we would go home and get as much sleep as we could and hope for no overnight emergency phone calls. Weekends were much the same minus the drop-offs and pick-ups at my office and Taylor’s daycare.
Take A Breath Boy
During the weeks Eric was in the NICU, we learned Eric did not have ROP, but he did battle several other conditions, including two brain bleeds and blood in his spinal fluid. Eric made the machines measuring heart rate and blood oxygen saturation sound like a slot machine hitting a jackpot several times a day due to him experiencing Apnea and Bradycardia. Apnea is a temporary pause (more than fifteen seconds) in breathing that is common in preterm infants. It often is associated with a decline in the heart rate, called Bradycardia. A drop in oxygen saturation as measured by a machine called pulse oximetry is called desaturation.
Wendy explained when Eric experienced an extreme desaturation event the NICU nurses would have to provide Eric supplemental oxygen using a blow-by technique. This technique required that a 100% oxygen flow be directed into Eric’s face. With the passing of each day, Wendy became more skilled at reading Eric’s body language and the monitors, and often could encourage Eric to take a breath before desaturation occurred by rubbing his back or squeezing his foot or hand, reducing the need for blow-by oxygen.
Wendy also became an expert feeder. Eric would take his bottle real slow and oftentimes start to turn blue during a feeding when he forgot to take a breath. Rubbing his back or squeezing his foot or hand typically is all it took to avoid a monitor-alerting desaturation event.
Most infants, as did Eric for the most part, outgrow the Apnea and Bradycardia condition by the time they leave the hospital for home. However, it was decided that Eric needed to use a monitor at home, and we were trained on how to use an oxygen bottle in case a blow-by was required. Before Eric could be released from the NICU, Wendy and I had to spend a night with Eric in a separate room with us. About this time a NICU nurse realized the monitor we would be taking home only provided visual alerts. Fortunately, a second monitor that provided audible sounds for desaturation warnings was located. Ultimately, with no further delays, on Christmas Eve Eric was released to come home with us with two monitors and an oxygen bottle. I am happy to report the oxygen bottle was returned full as Eric never required a blow-by once at home.
